
By Alexander Gelfand, for the Johns Hopkins School of Public Health Magazine.
© Johns Hopkins University
The powerful genome-editing technology known as CRISPR-Cas made headlines this year—partly because many leading biologists called for a moratorium last March against using it to modify the genomes of human embryos, only to discover in April that Chinese scientists had already done just that.
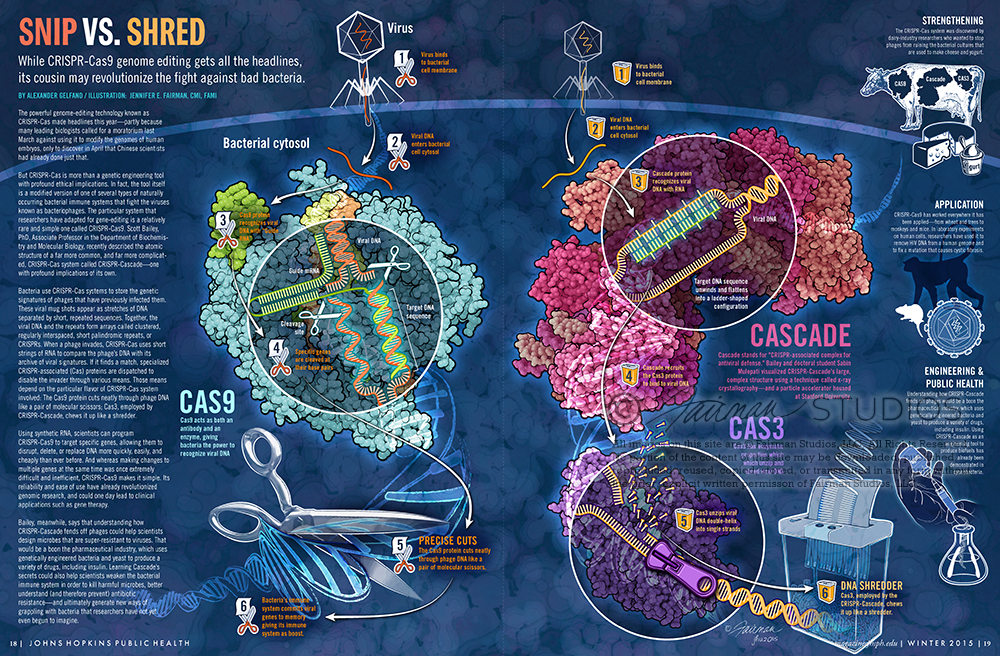
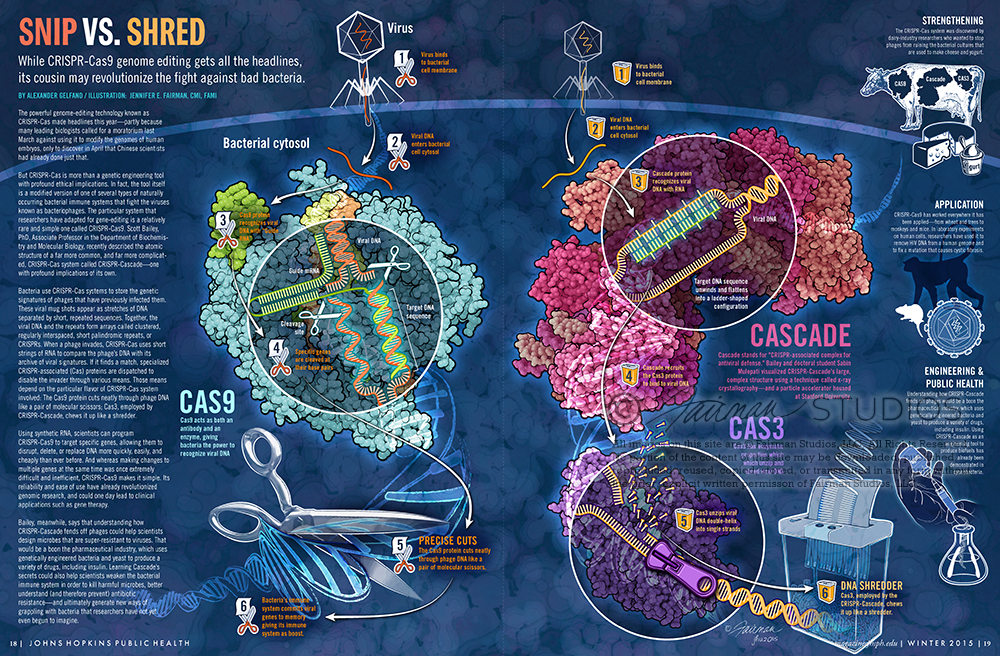
But CRISPR-Cas is more than a genetic engineering tool with profound ethical implications. In fact, the tool itself is a modified version of one of several types of naturally occurring bacterial immune systems that fight the viruses known as bacteriophages. The particular system that researchers have adapted for gene-editing is a relatively rare and simple one called CRISPR-Cas9. Scott Bailey, PhD, Associate Professor in the Department of Biochemistry and Molecular Biology, recently described the atomic structure of a far more common, and far more complicated, CRISPR-Cas system called CRISPR-Cascade—one with profound implications of its own.
Bacteria use CRISPR-Cas systems to store the genetic signatures of phages that have previously infected them. These viral mugshots appear as stretches of DNA separated by short, repeated sequences. Together, the viral DNA and the repeats form arrays called clustered, regularly interspaced, short palindromic repeats, or CRISPRs. When a phage invades, CRISPR-Cas uses short strings of RNA to compare the phage’s DNA with its archive of viral signatures. If it finds a match, specialized CRISPR-associated (Cas) proteins are dispatched to disable the invader through various means. Those means depend on the particular flavor of CRISPR-Cas system involved: The Cas9 protein cuts neatly through phage DNA like a pair of molecular scissors; Cas3, employed by CRISPR-Cascade, chews it up like a shredder.
Using synthetic RNA, scientists can program CRISPR-Cas9 to target specific genes, allowing them to disrupt, delete, or replace DNA more quickly, easily, and cheaply than ever before. And whereas making changes to multiple genes at the same time was once extremely difficult and inefficient, CRISPR-Cas9 makes it simple. Its reliability and ease of use have already revolutionized genomic research, and could one day lead to clinical applications such as gene therapy.
Bailey, meanwhile, says that understanding how CRISPR-Cascade fends off phages could help scientists design microbes that are super-resistant to viruses. That would be a boon the pharmaceutical industry, which uses genetically engineered bacteria and yeast to produce a variety of drugs, including insulin. Learning Cascade’s secrets could also help scientists weaken the bacterial immune system in order to kill harmful microbes, better understand (and therefore prevent) antibiotic resistance—and ultimately generate new ways of grappling with bacteria that researchers have not yet even begun to imagine.
The CRISPR-Cas system was discovered by dairy-industry researchers who wanted to stop phages from ruining the bacterial cultures that are used to make cheese and yogurt.
CRISPR-Cas9 has worked everywhere it has been applied—from wheat and trees to monkeys and mice. In laboratory experiments on human cells, researchers have used it to remove HIV DNA from a human genome and to fix a mutation that causes cystic fibrosis.
Cascade stands for “CRISPR-associated complex for antiviral defense.” Bailey and doctoral student Sabin Mulepati visualized CRISPR-Cascade’s large, complex structure using a technique called x-ray crystallography—and a particle accelerator housed at Stanford University.

This illustration was created for a May 2015 AFP article reviewing the diagnosis and management of GAD and PD in the primary care setting. While GAD and PD can develop among children and adolescents, diagnosis and care for these younger populations requires special considerations beyond the scope of this review.
Generalized anxiety disorder (GAD) and panic disorder (PD) are among the most common mental disorders in the United States. Frequently encountered by primary care physicians, both GAD and PD can negatively impact a patient’s quality of life and disrupt important activities of daily living. Evidence suggests that missed- and misdiagnosis of GAD and PD are high, with symptoms frequently ascribed to physical causes. The diagnosis of GAD and PD requires a broad differential and caution to identify confounding variables and co-morbid conditions. Screening and monitoring tools can be used to help make the diagnosis and monitor response to therapy. The GAD-7 and the Severity Measure for Panic Disorder are both available without cost. Successful outcomes may require a combination of treatment modalities tailored to the individual patient. Treatment frequently includes medications such as selective serotonin reuptake inhibitors (SSRIs) and/or psychotherapy, both of which are highly effective. Among psychotherapeutic treatments, cognitive behavioral therapy (CBT) has been studied widely and has an extensive evidence base. Benzodiazepines are effective in reducing symptoms of anxiety, but their use is limited by risk of abuse and side effect profiles. Physical activity can reduce symptoms for both GAD and PD. A number of complementary and alternative treatments are frequently used; however, evidence is limited for most. Several commonly used botanicals and supplements can potentiate serotonin syndrome when used in combination with antidepressants. Medication should be continued for 12 months to prevent relapse.
 Generalized anxiety disorder (GAD) and panic disorder (PD) are among the most common mental disorders in the United States (US). Frequently encountered by primary care physicians, the hallmark feature of GAD is excessive, out-of-control worries; for PD, it is recurrent and unexpected panic attacks. Both GAD and PD can negatively impact a patient’s quality of life and disrupt important activities of daily living. Missed- and misdiagnosis of GAD and PD are high, with symptoms frequently ascribed to physical causes.
Generalized anxiety disorder (GAD) and panic disorder (PD) are among the most common mental disorders in the United States (US). Frequently encountered by primary care physicians, the hallmark feature of GAD is excessive, out-of-control worries; for PD, it is recurrent and unexpected panic attacks. Both GAD and PD can negatively impact a patient’s quality of life and disrupt important activities of daily living. Missed- and misdiagnosis of GAD and PD are high, with symptoms frequently ascribed to physical causes.

This illustration was created for the January 15, 2015 feature article for American Family Physisician about Wound Care. This article reviews common questions associated with wound healing and outpatient management of minor wounds:
BROOKE WORSTER, MD; MICHELE Q. ZAWORA, MD; and CHRISTINE HSIEH, MD, Thomas Jefferson University, Philadelphia, Pennsylvania
Am Fam Physician. 2015 Jan 15;91(2):86-92.
 Patient information: See related handout on wound care, written by the authors of this article.
Patient information: See related handout on wound care, written by the authors of this article.
Lacerations, abrasions, burns, and puncture wounds are common in the outpatient setting. Because wounds can quickly become infected, the most important aspect of treating a minor wound is irrigation and cleaning. There is no evidence that antiseptic irrigation is superior to sterile saline or tap water. Occlusion of the wound is key to preventing contamination. Suturing, if required, can be completed up to 24 hours after the trauma occurs, depending on the wound site. Tissue adhesives are equally effective for low-tension wounds with linear edges that can be evenly approximated. Although patients are often instructed to keep their wounds covered and dry after suturing, they can get wet within the first 24 to 48 hours without increasing the risk of infection. There is no evidence that prophylactic antibiotics improve outcomes for most simple wounds. Tetanus toxoid should be administered as soon as possible to patients who have not received a booster in the past 10 years. Superficial mild wound infections can be treated with topical agents, whereas deeper mild and moderate infections should be treated with oral antibiotics. Most severe infections, and moderate infections in high-risk patients, require initial parenteral antibiotics. Severe burns and wounds that cover large areas of the body or involve the face, joints, bone, tendons, or nerves should generally be referred to wound care specialists.
Family physicians often treat patients with minor wounds, such as simple lacerations, abrasions, bites, and burns. This article reviews common questions associated with wound healing and outpatient management of minor wounds. More chronic, complex wounds such as pressure ulcers1 and venous stasis ulcers2 have been addressed in previous articles.

Creating cover art and illustrations for MCP, by Rajendrani Mukhopadhyay: ASBMB Today, January 2014
�The way Fairman worked on the art for the MCP special issue on posttranslation modi�cations was typical for any project she does. She met with Gerald Hart of Johns Hopkins University, the MCP associate editor overseeing the issue, and ASBMB’s publications director, Nancy Rodnan, whose idea it was to hire a professional medical illustrator. Hart explained the science in the various articles. With input from Mary Chang, MCP’s managing editor, the group focused on the images that were either schematics or illustrations. �They left alone the images that were captured by a camera or a computer.
“One of the things that I strived to do for this journal was to come up with a consistent style,” explains Fairman. For elements that came up repeatedly, such as ubiquitination, acetylation, proteins and organelles, Fairman established a style so that all of the �figures throughout the special issue had the same look and feel. Fairman also says she stuck to scientific conventions as much as possible in terms of colors and symbols. “For example, thinking back to my time in organic chemistry in undergrad, in the little molecular model set, oxygen is usually red, carbon is black, and hydrogen is white,” she says. “Whenever we create any visual, we have to keep in mind who the audience is. Because MCP has a scientifi�c audience, I’ve tried to come up with conventions that people are used to seeing.”
Fairman says it can be a challenge to �figure out what should be kept in and left out of an illustration. She had a difficult case with one of the �figures from the MCP special issue. “�e illustration shows a really complicated mechanism, where these different proteins on the cell membrane, endoplasmic reticulum, nucleus, all the different organelles, are interacting with each other,” she says. “Instead of showing every single protein in its correct configuration, the best thing to do to drive home the message is to use color coding. Not worry so much about what those proteins actually look like but focus more on what they do.”
With the cover, Fairman took another tack, because the cover has a different role than �figures in the scienfiti�c articles. �The inspiration for the cover art came from �figure 1 in the article by Corina Antal and Alexandra C. Newton at the University of California, San Diego, on the dynamics of lipid second messenger phosphorylation. “�e cover isn’t necessarily meant to show the whole mechanism in a way that the readers will completely understand it,” says Fairman. “It is supposed to engage them and bring them into the journal, wanting to read that featured article.”

This editorial illustration was created for a July 2014 cover of American Family Physician. The image summarizes Constipation in Children.
Childhood constipation is common and almost always functional without an organic etiology. Stool retention can lead to fecal incontinence in some patients. Often, a medical history and physical examination are sufficient to diagnose functional constipation. Further evaluation for Hirschsprung disease, a spinal cord abnormality, or a metabolic disorder may be warranted in a child with red flags, such as onset before one month of age, delayed passage of meconium after birth, failure to thrive, explosive stools, and severe abdominal distension. Successful therapy requires prevention and treatment of fecal impaction, with oral laxatives or rectal therapies. Polyethylene glycol–based solutions have become the mainstay of therapy, although other options, such as other osmotic or stimulant laxatives, are available. An increase in dietary fiber may improve the likelihood that laxatives can be discontinued in the future. Education is equally important as medical therapy and should include counseling families to recognize withholding behaviors; to use behavior interventions, such as regular toileting and reward systems; and to expect a chronic course with prolonged therapy, frequent relapses, and a need for close follow-up. Referral to a subspecialist is recommended only when there is concern for organic disease or when the constipation persists despite adequate therapy. (Am Fam Physician. 2014;00(0):000-000. Copyright © 2014 American Academy of Family Physicians.)
SAMUEL NURKO, MD, and LORI A. ZIMMERMAN, MD, Boston Children’s Hospital, Boston, Massachusetts, Evaluation and Treatment of Constipation in Children and Adolescents, Am Fam Physician.

This editorial illustration was created for a May 2014 cover of American Family Physician. The image summarizes Unintentional Weight Loss in Elderly.
Elderly patients with unintentional weight loss are at higher risk for infection, depression and death. The leading causes of involuntary weight loss are depression (especially in residents of long-term care facilities), cancer (lung and gastrointestinal malignancies), cardiac disorders and benign gastrointestinal diseases. Medications that may cause nausea and vomiting, dysphagia, dysgeusia and anorexia have been implicated. Polypharmacy can cause unintended weight loss, as can psychotropic medication reduction (i.e., by unmasking problems such as anxiety). A specific cause is not identified in approximately one quarter of elderly patients with unintentional weight loss. A reasonable work-up includes tests dictated by the history and physical examination, a fecal occult blood test, a complete blood count, a chemistry panel, an ultrasensitive thyroid-stimulating hormone test and a urinalysis. Upper gastrointestinal studies have a reasonably high yield in selected patients. Management is directed at treating underlying causes and providing nutritional support. Consideration should be given to the patient’s environment and interest in and ability to eat food, the amelioration of symptoms and the provision of adequate nutrition. The U.S. Food and Drug Administration has labeled no appetite stimulants for the treatment of weight loss in the elderly.
Unintentional weight loss in the elderly patient can be difficult to evaluate. Accurate evaluation is essential, however, because this problem is associated with increased morbidity and mortality. When a patient has multiple medical problems and is taking several medications, the differential diagnosis of unintentional weight loss can be extensive. If the patient also has cognitive impairment, the evaluation is further complicated. To successfully address this problem, the family physician needs to understand the normal physiologic changes in body composition that occur with aging, as well as the consequences of weight loss in the elderly patient.
GRACE BROOKE HUFFMAN, M.D., Brooke Grove Foundation, Sandy Spring, Maryland Am Fam Physician. 2002 Feb 15;65(4):640-651.